This is Chapter 13 of 50 in a summary of the textbook Handbook of Healthcare Delivery Systems. Go to the series index here. Listen on YouTube Playlist, or search your podcast app: Gregory Schmidt
Chapter 13 Summary
Toward More Effective Implementation of Evidence-Based Practice: Relational and Contextual Considerations
Chapter Authors
Priscilla A. Arling - Butler University
Rebekah L. Fox - Texas State University
Bradley N. Doebbeling - Indiana University School of Medicine
Some Commentary
This chapter is not very good. It provides the general platitudes about what is wrong with the healthcare system, and then provides some very wishy washy high level concepts on how evidence-based practice can be implemented better.
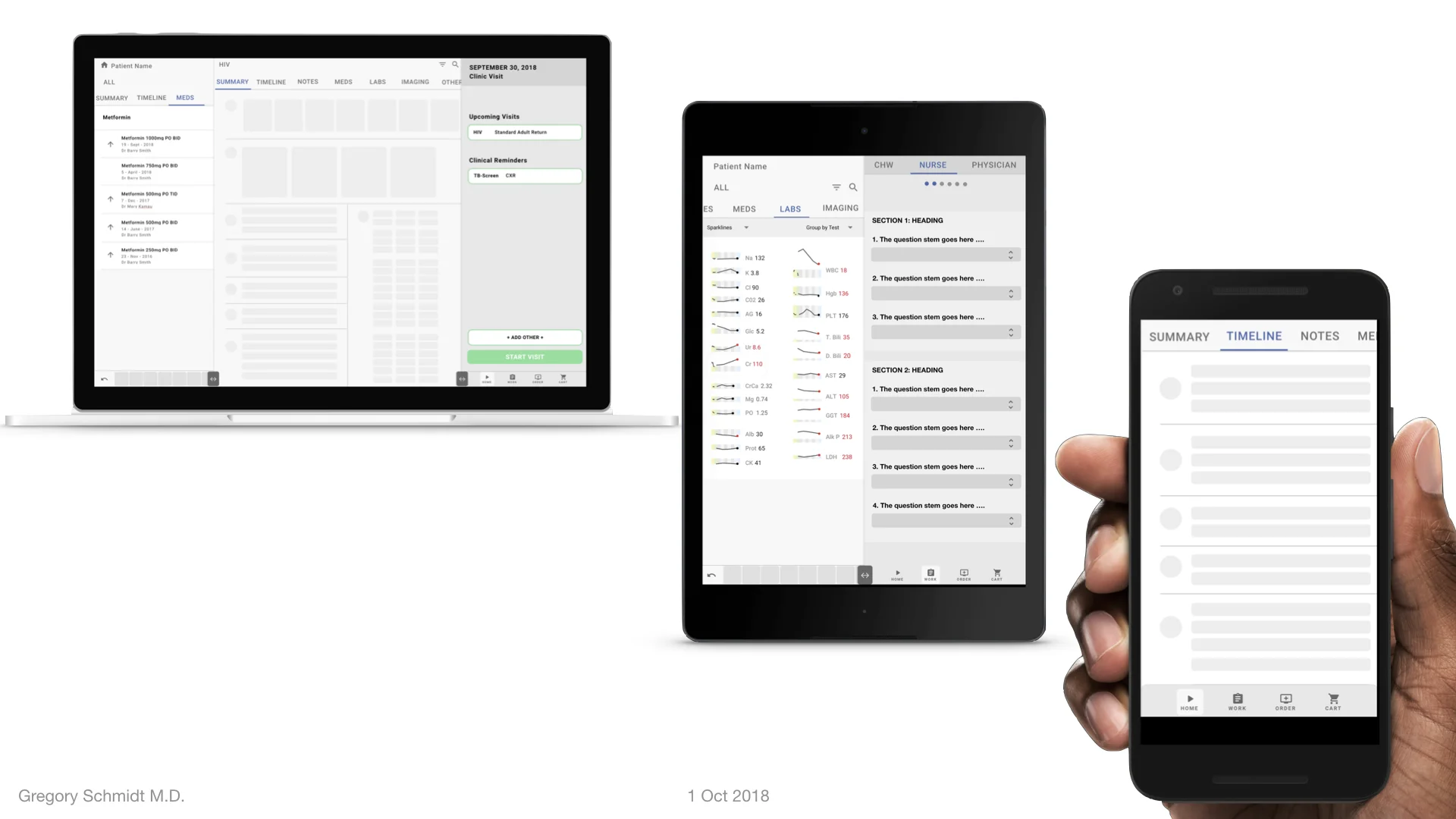
I would have preferred to read case studies about how evidence-based practice has been implemented rapidly and scaled. What are the social / cultural / and technologic considerations that made that a success. I’d also like to have read about electronic medical records that do evidence-based practice reminders well. To conclude, some case studies outside of healthcare where research innovations make it quickly to the factory / shop / or field would have been a good comparison.
1. Evidence Based Practice
The chapter opens with the standard concerns.
The numbers show the United States is missing the mark. Around half of patients receive necessary care, and under half of physicians use “recommended processes of care” (whatever that means).
An example of systems failures: in America those with HTN 70% are diagnosed, 60% are treated, and 30% are controlled.
“It is estimated that 30-40% of healthcare expenditures, or $600 billion, is spent annually on costs associated with ''overuse, underuse, misuse, duplication, system failures, unnecessary repetition, poor communication and inefficiency” (Ried et al., 2005 pp3-4)”
Fragmentation among different clinical settings (what I’ll call horizontal), and lack of communication between the multiple levels of care around the patient (what I’ll call vertical). All of these horizontal and vertical layers do not coordinate or interact and work to create a 3-Dimentional ball of chaos.
PARiHS Framework
The chapter notes the PARiHS framework relies on integration of:
Evidence: research evidence, clinical experience, patient preferences, routine data
Context (of place evidence is implemented): culture, leadership, and evaluation
Facilitation: what is to change people’s attitudes and behaviours based on the evidence and context
2. Social Capital Theory
Text defines social capital as
Obligations, expectations, and trustworthiness: people trust each other when they do things for each other, and that it will eventually be reciprocated
Information channels
Norms and Sanctions
2a. Social Network Aanlysis (NSA)
Social Network Analysis is the mapping of people in an organization and their relationship to each other. Each person is a node, and their relationship a line. Some people may end up having thicker lines as they are connected to many people.
Information may disseminate through networks that have higher density (more connections). Some nodes/people are ‘influencers’ and making them the disseminators of new evidenced based practices may help increase the transmission of data through the network.
2b. Communities of Practice (CoPs)
A Community of Practice is simply a group of individuals united around a common interest. The interest can be a topic, task, or issue. Group membership is voluntary and members learn from each other, and are able to share both explicit and tacit knowledge on the subject