Medical Revolution 50 years early | Dr Larry Weed's Original 1971 Lecture
If you prefer to watch, listen to the 15 minute post summary:
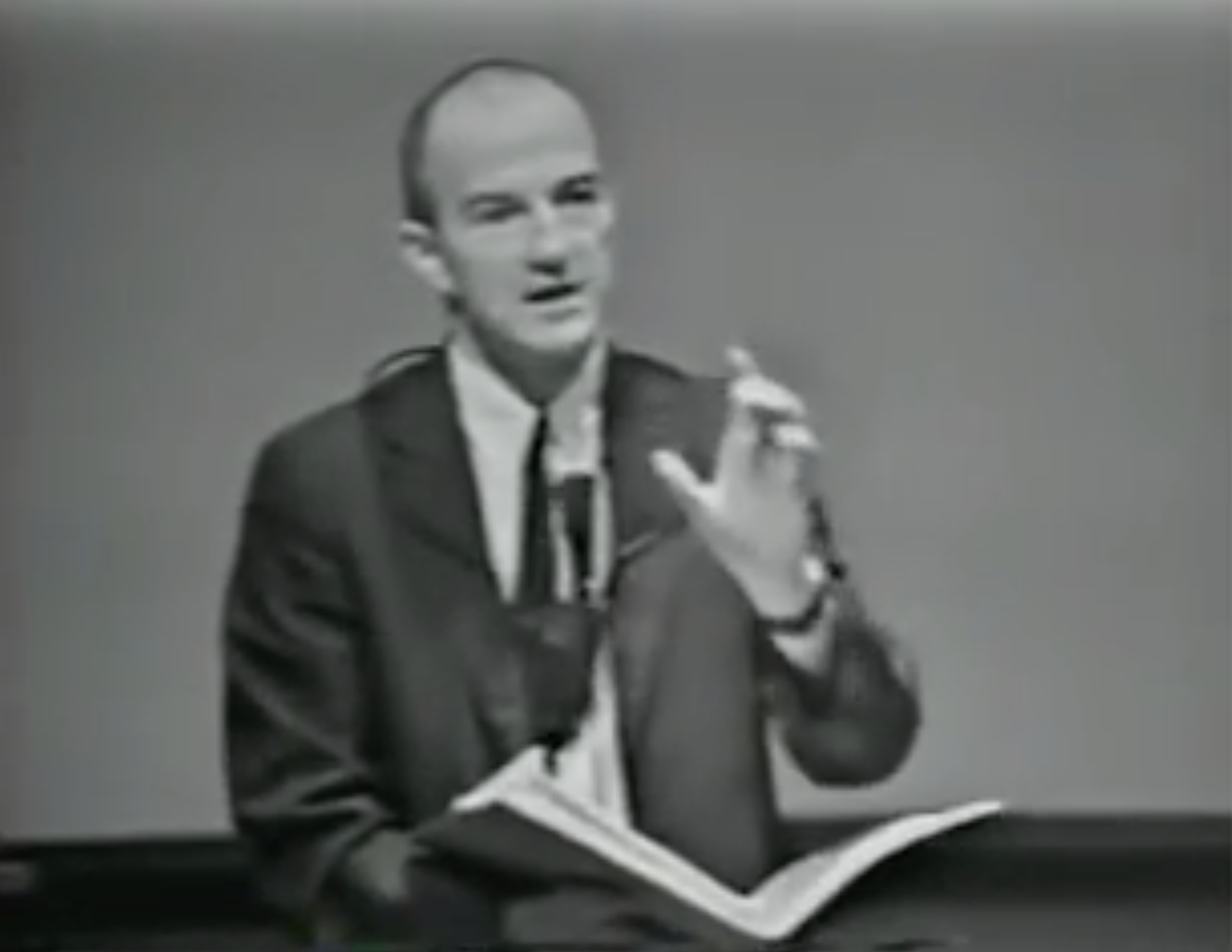
But the real point of this post is to direct you to the original 1971 lecture below by Dr Larry Weed.
It explains the core issues and mistakes of medical care with great accuracy, while being hilarious and scathing all at the same time.
Every overnight success is a story 25 years in the making. Everyone notices something when an exponential curve starts taking off, but never noticed it prior. In the case of the revolution happening in medical informatics and computer aided diagnosis at the moment, this is a story well over 60 years in the making.
Dr Larry Weed tried to shine light into the field of medicine over half a century ago and show us how sloppy, unscientific, and un-’artistic’ we actually were. Many of his observations went unheeded. Until now.
He knew what was coming. In this lecture he states, “…and now when the computer people move in… and the non-medical people move in, they can hardly believe what they see. And there is a crisis of major proportions.”
Dr. Larry Weed Internal Medicine Grand Rounds (Recorded 1971)
Delivered at Emory University. 54 minutes.
This video was preserved & uploaded by Dr Weed’s pupil Dr. Art Papier. Dr Papier runs VisualDx, a very innovative company using machine learning aided diagnosis, inspired by the thought of dr Weeds. Their tool is kind of like a Palantir for medicine.
Some memorable quotations
On the “art of medicine” “Where is the art of medicine going to go with all of this? …art is Hemingway spending three weeks on a single paragraph. Its Bach recording in detail everything he did…it is not a scribble in the middle of the night…It's not saying, ‘I took good care of her’, while leaving absolutely no trail for us to ever find out if you did or did not. We debase the word art itself when we call what we've been doing art… And it's not science… so we have to extremely be careful when we defend what we're doing… We don't want to reveal to others that we didn't even get a liberal arts education, as Stravinsky says, ‘art is nothing more than placing limits and working against them rigorously’… And if you refuse to place them and to try and work within them, but flay out - you do not have art. You have chaos. And to large extent, that's what we have.
On patient resilience and medical diagnostic error, “Well you realize I'm sure, that the Lord and the chiropractors can get 85 per cent of these people better. The only reason you run these fantastic establishments [hospitals] is to get that other 10%. The only reason you have a Professor of Medicine is to pick up that final 2 per cent.”
On patient centred care: “Now… what are you going to tell the patient? And no place in American records do we have an organized approach to [chart] what we're going to tell the patient. Under that hypertension did you tell her it was serious or not serious? How are you going to study it or whether you're not going to study it? ” [note: this still is not part of the medical record]
On the fallibility of doctors “…That's the way interns and residents and doctors are. If they work perfectly it would be one thing, or if they didn't work at all. But we half work. We half guess. We half understand. We half know.”
On keeping accurate records “…But the reason we don't like to do it is because your faults are so obvious. Your mistakes are so obvious. The lack of purity of your approach is so obvious. You can't stand it, so you say it's “unimportant” or “is not scientific” or “that not why I came into medicine.” Your cowards. It’s perfectly clear that's what the problem is.”
On Source-Orientated medical records: ‘Why do you put the x-ray of the ear with the x-ray of the hip? What’s the ear got to do with the hip? Why did you have all those ear cultures with those urine cultures? Is she urinating in her ear? What are you doing that for?”
On Medical Data & Medical Thought: “This is not an idle discussion of little technical bookkeeping details. The practice of medicine is the way you handle data and think with it. And the way you handle it determines the way you think. …the very structure of the data determines the quality of the output. This is what's so hard for medicine to accept.”
On physician memory: “Well, then you might say, ‘Why don't you call up the doctor and ask him?’ I'd say, ‘but that note was two months ago. You can't be serious.’
You don't say to a teller in the bank, ‘you remember Mr. Jones came in two weeks ago and he put…how much money did he put on the shelf?’ If she answers you would think she is crazy
… But in the medical faculty, writing discharge summaries three weeks later, preoperative notes after the operation, someone writes all their progress notes on Sunday morning. That's fiction, it's not science. “
On quality in medicine: “…if you can’t audit a thing for quality, it means you do not have the means by which to produce quality. They've inextricably entwined. If you can't evaluate what you're doing, then it’s a very serious possibility that you do not know what you're doing.”
On systems: “…when someone says, “I take care of that patient, I'm her doctor” - that's fraudulent. No one points to a Pontiac and said, “I made that car”. A system makes that car… It's like Henry Ford saying I personally am going to make an automobile for everyone in the population. I don't believe in systems and assembly lines. I'd rather buy a personal touch on it. He will make an automobile for two or three people, a year the other 200 million will have none. And that is the basis for a revolution.
… This [the record] is the basis for a system. The records has to be. You can write a check in Atlanta on a New York Bank why, because there's a system. And it's known throughout”
On the Problem Orientated Medical Record
1. The Database - must be complete and the same every time. “And if you don't have time to do it get paramedical care people to do it, they will do it better anyway. And they will write it up so you can read it.
… You use computers with branching logic questions
… Do whatever you have to do, but get the database, and get it every time.
… We found in the action room [ER], with a questionnaire that had 32 questions and we got the vital signs and we did it paramedical personnel. It took between 9 - 11 minutes. We found that the doctors were missing an average of 5.2 problems per patient. And some of them were quite serious.”
2. The Problem List - “I'm not interested in what the impression is, I'm interested in what do you know to be the problem. And no ambiguity about it.”
…In a chart I see “?organic heart disease”… I say, well, what's the problem?… “she's that one with the funny Cardiogram.”… He said, '“well, jeez… but you don't honestly want me to put down ‘problem number four, funny looking EKG. Now, do you?’”. And I said, “yes doctor. If that's the level at which you understand the problem put it down that way.” If that's the level in which your care is being given, there is nothing to be ashamed of about that… All you have to do is be honest
3. The Plan “…No one should ever be able to write an order without coupling it with a problem.
… It was like walking into a room and people were throwing darts, and you say “where is the target?” … “Wherever the dart lands.”
3 parts to the plan: (a) rule outs and investigations, (b) treatments, (c) what did you tell the patient
4. Follow Em - “Now what I'm saying is, that a doctor has to be a guidance system. He is not an Oracle that knows answers. And once he accepts the concept of being a guidance system, then he knows that the data system is the basis from which all his work must take place.”
Transcript of Larry Weed’s 1971 Grand Round’s Lecture
My emphasis in bold added.
The transcript doesn’t do justice to his presentation. Though may be helpful if you are trying to find an approximate quotation.
Introduction
Its good for me to be here. I don't know if whether when I'm done, you will think it's good that I was here. I can be a real hit and run driver. I don't have to stay here, and If I'm lucky, I won't get sick in Atlanta. Because once you antagonize somebody and you get sick in front of them. You're never quite sure whether you're safe or not. But what TV said, you shouldn't get sick in America anyway.
But now what I'd like to do is go at this problem, not at the point of view of the record. I mean we are not really taking care of records we are taking care of people, and we're trying to get across the idea that this record cannot be separated, from the caring of that patient.This is not something with the practice of medicine over here, and the record over here.
This is the practice of medicine.It's intertwined with it. It determines what you do in the long run. You're a victim of it, or you're a triumph because of it.
The human mind simply cannot carry all the information about all the patients in a practice without error. And so the record becomes part of your practice. And when you hear someone say, “well, I know lots of good practitioners…the best surgeon in the place…he doesn't keep any records at all.”
How do you know he is so good? Because he talks fast? Because he operators fast? We have to see the record. How many gastrostomies has he done? How many haven't had any infections? What do the wounds look like? How many have dumping syndromes? How many have died? How many got infections? Without a record, we're not going to believe him. It's like asking somebody his golf score three years ago without it written down. It will always come out better than it actually was.
(1:56) All right now, we've got to look at the record and if this represents practiceand you walk into a place like this, you'd say, “Well, I'd like to see how medicine is doing here?” You know, people say it's a very good place or very poor place. Well, how do you know?
Reading the chart, looking for the patient’s problems
Well, let's see what the patient's problems are? I picked this [chart] out of your clinic this morning. If you tell me what the problem is, and I have a few minutes, I will either know myself or I'll go to books or I'll go to experts and most will say that's pretty good standards for that problem. But I would have to know the problem.
Well, the first sheet is a little sheet here, that says, Oakland Avenue something… then Phenobarbital addict, impression, probable addiction… and a then a scribble here, then there's a blue sheet…. and I keep leafing through all this stuff…and then there's an x-ray report, ‘normal brain scan’…. wow they really didn't do that for Phenobarbital addiction, I don't think… And I am leafing through this, and I'd say, “Jeez, I'd like to know where the problems are”. And you say, Oh, come on now Doctor Weeds. Pull yourself together. Let's not try to make a big thing out of this record business. Just because you happen to be interested in records.
(3:13) Well, you know, I'm interested in nucleic acids chemistry. I've have been a biochemist lot longer than I have been fussing around in clinical medicine, and it's not that I'm so interested in records. I'm interested in medicine. I have used these to find out what was going on and it's gotten my absolutely, you know, climbing the wall.
I could set it [the record] aside like I used to, and say, “well, never mind the record. I'll tell you all I know about pyelonephritis”. But that has nothing to do with her. That's grand rounds on me. That isn't what you come for. So I'd say, “I would like to know the problems”. He said, “well, there's the end of the work up. Find the first work up and you will find the problem”. So I come to one, and I read through this, “impression: CVA, number two: extreme anxiety neurosis. Was that all the problems? All right, if that's all the problems we can see how you diagnosed it, and you did for it. And see if that's good care for CVA.
So I’m thumbing through here and it says blood pressure 180 over 100 or 98. Thorazine, are they giving Thorazine for a stroke? No they're giving that for the anxiety maybe…I'm not quite sure. Then what's all this SSKI? Then here, LE prep times three - for anxiety or a stroke? Then x-rays of the left hip and pelvis. Then he might say, “oh well don't get excited, she probably fell out of bed.” Did she? I don't know…. Urinary tract infection, honest to God, now they're x-raying the left shoulder, and the left hand… Next one, Impression, same patient, chronic obstructive lung disease, personality disorder… Now then I go to the lab sheets, and you know what I see: PVI's, BUN's, serum sodiums, and one sheet over there a whole bunch of electrolytes in a row. And you don't do serum sodium and all those electrolytes every day for stroke. You don't do them for anxiety. There must be another problem.
(5:32) Well, now, I can't audit it. I don't know, whether you're giving good care of the problem. I don't even know whether you're finding all the problems. And if problem number one is hypertension and problem number five is depression and you're giving amitriptyline for problem number five for the depression that's all right in itself. But that antagonizes guanethidine if you stop the amitriptyline. And then they've upped the dose of guanethidine, and then she has a shock and hits her head on the bathtub, and then she comes in for a subdural hematoma: that's your fault. But I can't find it because it's too hard to interpret this. You can't look at the management of a single problem without knowing the context of all the problems. Yes, she should have the hip pinned, but not today because number one is heart failure. Yes, she should have fluids restricted, but number three is an azotemia. Yes, she should have lots of fluids…it’s tough…its tough. And you shouldn't have to spend a second finding what are all the problems.
Source Orientated Medical Record
(6:34) Now what kind of a record have we got here? We have got a source-oriented record. It's not a problem-oriented record. What I mean by that is this, in a source oriented record, you put all the lab data together, you put all the x-rays together, and you put all the temperature sheets together, you've got all the nurses notes together, you have all the doctors’ notes together.
And I would say, “I like to know what you're doing for the ladies ear.” Well, there is the temperature, might have to with the otitis. And then I read the notes by the doctors and the progress notes. If you read some of these progress notes…”doing well”… “home tomorrow”… ”phenobarb”… ”acute arthritis”… “shoulder swollen”… “ECS 600 milligrams”… “RTL”… you know…ABC, XYZ.
And its all -- it flows it's a single paragraph: the elbow, urinary tract. It’s a series of things. Now, that's the doctor’s notes. Now you have the white counts and the serum sodiums and the urines together. Then you x-ray of the ear, with the x-ray of the chest, with an x-ray of the hip. And I'd say, “what are you doing that for?”
Why do you put the x-ray of the ear with the x-ray of the hip? What’s the ear got to do with the hip? “Well, nothing but we like to put those together.”
Why did you have all those ear cultures with those urine cultures? Is she urinating in her ear? What are you doing that for?
(8:08) Now when people source-orient data, you appear very unscientific. But it's even worse than the appearance. It's the very essence of the practice of medicine. This is not an idle discussion of little technical bookkeeping details. The practice of medicine is the way you handle data and think with it. And the way you handle it determines the way you think.
Once you get over a period of time with multiple variables the very structure of the data determines the quality of the output. This is what's so hard for medicine to accept.
They can't say things like, “I know lots of good doctors that don't keep good records.” They can't be separated that way. Now you might say, “well, you could figure out what's wrong with that ear if you wanted to. You could sit out and read the whole record”. Well with 200 million people, and to get quality I might spend three hours. But even then I couldn't do it. It would be impossible. Because I would be guessing. I’d come to the order sheets…like this order sheet.. it has all these orders. Now I see Penicillin on it, I wouldn't be sure whether if that's for the urinary tract infection, pneumonia, or the ear. It doesn't say…
Pitfalls of recall from memory
(9:49) I see a brain scan, I could guess that maybe that's for the stroke or I don't know or maybe he is worried about a subdural, or maybe he's worried about a tumor. I don't know. I'm guessing. Well, then you might say, “Why don't you call up the doctor and ask him?” I'd say, “but that note was two months ago. You can't be serious.”
You don't say to a teller in the bank, “you remember Mr. Jones came in two weeks ago and he put…how much money did he put on the shelf?” If she answers you would think she is crazy.
If I had a technician who read the specs on a thermometer on Wednesday and wrote the numbers in a notebook on Thursday, I would fire her. And I would get complete support in the basic science faculty for doing so.
But in the medical faculty, writing discharge summaries three weeks later, preoperative notes after the operation, someone writes all their progress notes on Sunday morning. That's fiction, it's not science.
Better you do not write anything at all than something that is not absolutely reliable.
Quality & auditing
(10:42) Alright. So a source-oriented record is essentially useless.
From the point of view of a rigorous audit. And mind you, if you can’t audit a thing for quality, it means you do not have the means by which to produce quality. They've inextricably entwined also. If you can't evaluate what you're doing, then it’s a very serious possibility that you do not know what you're doing? And if you've never defined your goal, and that is true in medicine. We have not.
The Problem Orientated Medical Record (POMR)
Now you will hear clinicians say, well we've always had good clinicians have always problem-oriented there records. Oh, no they haven't. Now let's look at the four phases of medical action.
Let's divide medicine into
1) This is the database - that is the first phase of medical action.
2) Now after you get some information you're going to formulate the problems, So you're going to make a problem list.
3) And after you get a problem list, you’re going to have a plan for each
4) And then you should follow each
Those should be titled and numbered progress notes.
Now you say, well, that's what good clinicians have always done. They've done a history, a physical and lab work, that's what the database is. And then they have made a list of impressions…we call it impressions, he calls it problems…no difference there. Then we had a plan, we wrote it in the order book. And then we wrote progress notes. What is so new about this? Well, let's take each one separately here.
POMR 1.1 The Database
(12:55) Let's take that database, you have a picture of that in your mind. Was that ever defined? That that problem list is determined by that database.
If all you know is her name, she doesn't have any problems. If you know her name with and blood pressure you may have one. If you know her name, and blood pressure, and do a pelvic you may have two.
So I would walk in here and I say, “what's the guaranteed database for these patients?”
Well, the intern does the history and physical. Well, you know what that means: some ask five allergy questions; some ask fifty-five; some ask five if they have one admission; they ask one if they have five admissions; and they ask none if they have seven admissions.
So the problem list is determined by: where ge train, what he is interested in, how many people came in last night, what the professor asked for - do we have a rheumatologist for the attending? That is not the way to run a shop.
If you want a guaranteed list of problems and deal with the list of problems in context, you better define the database and you should get it every time time.
And if you can't get a complete database of people who have nails in their foot, you say, fine for these complaints like a nail in the foot…a broken arm…a person with a penal drip or gonorrhea… or something in his eyes – for them we get what we call a mini database.
For episodic care, we do not get the whole database. If you have a nail in the foot ask these three questions, we will feel for your lymph nodes and your groin or something, we will always give the TAT, we do that much.
But for comprehensive care, for someone with hypertension, or weight loss, or headaches, we do this. We have branching logic questions. We always do this on physicals. We get for this age group this lab work: for the 40-year-old we will get triglycerides, and such. X- Rays you're done with this frequency. PAP's are done with this frequency.
POMR 1.2 The Database - task shifting
(14:52) And people say, “well…who would have time to get all of that?” Well, then get somebody else to do it. You’ve got to set the goal and then stick to it.
And if you don't have time to do it get paramedical care people to do it, they will do it better anyway. And they will write it up so you can read it.
But you-- for instance in our clinics, the house officers were telling me this morning, “Oh, well, we don't have time, it's awfully busy in that clinic. We don't have time to get pelvic.” They have an excuse for everything. So what did I do? When patients came in the front door, when they registered if they are female they go to the fifth floor. We train nurses to do the pelvic exam, the rectal exam, the belly exam, the breast exam, the thyroid exam. It was done in an organized way, checked off, and then they were checked out by the Professor of Ob-gyn.
You know, as well as I do that they found much more than what was being found in the medical clinic. In the medical clinic, they either didn't get a pelvic or half of the time the fellas who did it might as well been sticking their fingers out the window; you know that as well as I do.
They [the medical officers] were never cleared in an organized way on these problems. Whereas when we taught the nurses, we ran them through 50, we check them out the systematic way. Yes, she's competent.
Database and the goal
(16:10) We took no risk on box number one, getting the database.
You use computers with branching logic questions. You can use mark sensesheets. You can use interviewers. Take these things and put them through a Selectric typewriter through the business office computer. Do whatever you have to do, but get the database, and get it every time.
We found in the action room, with a questionnaire that had 32 questions and we got the vital signs and we did it paramedical personnel. It took between 9 and 11 minutes. We found that the doctors were missing an average of 5.2 problems per patient. And some of them were quite serious.
They were seeing in the patient what they wanted to see. And they played Sherlock Holmes too early. They would ask one question, and the next question will be determined by the first question, because that's where they were brought up in a CPC sort of an atmosphere. “What do you think off next doctor?” You know, let's put two men on the chessboard, and move one and we will decide we will put the others on. Oh, no, you won't. You'll put them all on. We'll look at the rules. And then we should start to play.
It's very arbitrary how much data you get before you start to think? And under pressure? If you let people get data in a Sherlock Holmes way, they get less and less data, and use more and more intuition. They draw conclusions more and more prematurely. This get people into more and more trouble. They always say they don't have time. In nine minutes. You can find out a fantastic amount of information if you were to just do it. Don't think just do it.
Now, people say yeah, but it's so arbitrary. Well, I know its arbitrary. Everything is arbitrary. A football field is arbitrary. It could be it could be a 150 yards long, it could be 75, and it could be a 100. But if you do not draw the line, you will not play the game, and you won't know how you're doing. Say suppose I'm running down the field and I fall down in the 15-yard line. And I get up and say, “Oh, that's a touchdown”, but by who's definition, “my own I'm tired today”.
Now that sounds absolutely ridiculous. But that's the way we practice medicine.Best ENT man in town hasn't listened to heart in 20 years that's his database. Then they'll say he never gets in trouble. Oh, maybe once out of 100 times, he took that lady up to the OR and took her larynx out and she happened to be in bad heart failure, she got an arrhythmia and she died, or something but he didn't know she was hypertensive.
Well, you realize I'm sure that the Lord and the chiropractors can get 85 per cent of these people better. The only reason you run these fantastic establishments is to get that other 10%. The only reason you have a professor of medicine is to pick up that final 2 per cent.
Now, so we know it's arbitrary, but you must define it.And once it's defined, once you realize you've fallen down the 15-yard line. You say that's a touchdown, and I say, no you don't get a score, you got to over that line. Oh, geez, don't I get some credit? “Gee, I've been fighting all the way down this the field for an hour and they battered me up and I'm exhausted. And then we're awful big guys who were on top of me. There is this guy down there in the medical clinic, he doesn't realize how big this.” I'm sorry, buddy if you don't go over the line you don't get credit.
Now once that's very clear your mind and the object is to get the data you'll finger out ways. Now, you will learn to think up forward passes and you'll go home and study up new plays because we're not going to change the game just because you're tired.
And you begin to improve this profession, but this profession is truly is a cottage industry. Everybody wondering around to define his own game. And when you're allowed to define your own game, you're a fool not to define it in a way that you're always a victor. Of course, the medical profession gets the appearance of being arrogant and independent. Anybody that's been allowed to defend his own game all his life, that's conducive to arrogance. He never has a defeat. He's always got a way out. She was too sick. She went sour. What does that mean?
POMR 2.0 - The Problem List
(20:43) All right. Now, that's the first phase. Now you look at the second phase here. You're going to get a problem list from the database. You say, well, we've always made a list of impressions. Did we ever do that any better than the database?
Well, in first place we use the word impressions. Now that was a terrible thing to do in the first place. If you use the word impression or what you think, you then have to have the person who wrote the chart with you when you interpret the chart because what he’s thinking is part ofit.
I'm not interested in what the impression is, I'm interested in what do you know to be the problem. And no ambiguity about it. Well on occasions people say, Well, I don't know. Jezz, Larry everything is black and white to you. You just put a number on things and so-- I don't know if its rheumatic heart disease or cardiomyopathy. I say, well, what do you know? Do you know of a physiological findings? For instance, if you don't know-- if he doesn't know the diagnosis, you know a physiological finding.
Do you know the diagnosis? No, but do you know physiological finding? Like heart failure.Well, yeah, I know, she is in heart failure. Well, then that's your problem doctor. If you knew it was rheumatic heart disease put it down, that's your problem. We might say, well, if you want me to be absolutely honest, I don't even know that. But what do you know for sure? Is it a symptom of a physical finding? Well, yes, I'm very sure she is short of breath,I can guarantee you Dr. Weeds if I take you in the room you may not agree its rheumatic heart disease, and you may not think its heart failure. But you'll agree she’s very short of breath. I don't know whether it's chronic obstructive lung disease or cardiac failure. She may have a piece of corn caught in her trachea for all I know. Well, that's the problem.
Or you might say, you know, I picked up his chart he's got a question mark, organic heart disease. I saw that on one of those charts. I say, well, what's the problem? Well, he doesn't remember. “Oh, Gee, we had a lot of admissions last night…Oh, yeah, she's that one with the funny Cardiogram.” You say, doctor, that was pretty risky, you never want to lose sight of the problem. If you haven't been here, and I had used that chart, I could spend an hour trying to find out what the problem was. And I would have to go through your laundry basket to find that EKG, that's risky. He said, well, jeez, it seems logical to me but you don't honestly want me to put down problem number four, funny looking EKG. Now, do you? I haven’t done a course in cardiology, and I just don't know everything. I just don't think we can be expected to know everything. And I said, “yes doctor. If that's the level at which you understand the problem put it down that way.”
If that's the level in which your care is being given, there is nothing to be ashamed of about that. There's no reason why you should know all about cardiology. An ophthalmologist doesn't. And you don't know all about Ophthalmology either. The neurologist doesn't know all about Endocrine disease. All you have to do is be honest. And I'll say, to you what's funny about it. And the dumbest person, instead of putting down funny cardiogram, we will take one second and say what's funny about it, and look at the readings, and say “those are U waves, they shouldn't be there”. So the problem is Number 3: U waves in cardiogram.
Now you can call up anybody in seconds in the middle of the night, and say when you see this patient. What's the problem? You read off the problem and say Number 3 is U waves. He would say get a potassium.. do this.. do this and I will be in. He is halfway there. You know-- after 30 seconds he is with you.
But if you say going out the door, and say, “hey, I got a lady who I think as a little heart disease. Would you see her and I will see if I can operate tomorrow?” You can go upstairs and pick up this record, you could be fumbling through it for half an hour and still not sure what's bothering him. So what you usually do is throw it on the desk and say to the nurse, “show me the patient.” And he wonders down and looks her over and your kind experiences so you sort of think she will kind of live through that operation. And you hold your breath, and its usually the end of it. No, it should be much more precise than that.
So we have defined problems. We've put down impressions.
Now, what else about the problem list? It wasn't kept up to date. I stumble over the facts of: arthritis, LE preps, hip x-rays, PVI's, CVA's. This lady has at least 10 problems. Now, what happens when I stumble over it in this way? I'm scared to death there's something that I'm missing. So then, when I find a couple important one, they were terribly important, now I panic and then I go back, and now I've got to read every word…I wonder what I’m missing. Because there scattered in the box in the middle of pages and at the end of lab sheets.
Whenever a new problem appears, it should go on that problem list, and that problem list should sit on the front of the record and it should be absolutely up to date. And we have to be ruthless with a doctor. Not who does the wrong or right thing for heart failure - only God knows what's right or wrong for some of these problems - it's very confusing. But you have to be ruthless with him if he does not keep the problem list up to date so that anyone in seconds can be in context and make intelligent decisions.
You know over and over again, you'll hear us say, I didn't know. Postoperative when everything is going wrong. Then we discover in the old record that she has had hyperthyroidism and no one gave her the thyroid pills. And we've got myxedema coma on the operating table. That is inexcusable. And it happens in every hospital in this country. Lymph nodes didn't get cultured, I didn't know. I didn't know. I couldn't get time to go to the operating room doctor. It can't be you that takes care of a patient alone.
When you see a head resident running around at night, he can't see all the patients coming in. That's fraudulent, he can't possibly be the intern for that many people. He either has a system he trusts or he is going to lose. And when he is most ruthless with the people under him is when they violate the system. Because the people are in the hands of the system. And when someone says, “I take care of that patient, I'm her doctor” - that's fraudulent. No one points to a Pontiac and said I made that car. A system makes that car. And even in the pre Flexner days, no one could take out cataracts, handle porphyria, diabetic ketoacidosis, perforated ulcers, and depressions. No one ever did those as well as they can be done. Of course, we want specialization. If you have a gallbladder problem that's is really tough, of course, you want to Cattel to do it. He has done 1000 of them. He was magnificent. You want that. If someone takes out your mother's cataracts, you want the feeling and he has done 100's of these and he does it magnificently with minimal chance of failure.
But if he is that good and focuses, will he be able to encompass everything. No, he will not. So you want people to be part of a system. You don't what a family practice program where you teach them to be superficial. A system that builds automobiles, and it's going to take care of people. If we don't recognize that simple fact, then there is going to be an awful lot of people that are not going to get cared for. And there will be out there 100,000 people in the middle of Chicago floating around Cook County getting less than adequate care. It's like Henry Ford saying I personally am going to make an automobile for everyone in the population.I don't believe in systems and assembly lines. I'd rather buy a personal touch on it. He will make an automobile for two or three people, a year the other 200 million will have none. And that is the basis for a revolution.
This [the record] is the basis for a system. The records has to be. You can write a check in Atlanta on a New York Bank why, because there's a system. And it's known throughout. But if you get a coronary in Atlanta and your records are in Chicago, just try finding things out the first 24 hours. Even if you called up and they got another record the girl in the record room, isn't she in the same position I was [flipping through chart] what did you want to know doctor? You probably wouldn't be able to get her the phone, but if you did, you're just wasting your money. She should be able to read off that problem list just like that.
POMR 3 - Plans
(29:56) All right. Now, what about the next phase of medical action, where we talked about the plans for each problem. What have we done there? Well, we have taken an order sheet and just scribble orders like that. Penicillin, BUN, side rails, phenobarbital, serum sodium daily. IPV tomorrow. And he would say, “do you think those sodiums every day are necessary?” I don't know. I don't know what you did them for. And I suppose if he had some fancy endocrine disorder- aldosteronism or something you were fooling with that might be sensible. If it's for flat feet that's a waste of money.
No one should ever be able to write an order without coupling it with a problem.
Now when you write plans then you have to think of them in three phases. You put down problem number one, hypertension. You'll find you will get a whole new spirit out of your nurses once you start dealing with problem-oriented records. They become part of the team, they know everything they're doing, and they know how one doctor does it differently, they ask why, they become more and more sophisticated. Before they were asked to go blindly, they put the penicillin on the sheet - they didn't know what it was for. They couldn't see if you're being consistent. Whether you agree with other infectious disease people.
It was like walking into a room and people were throwing darts, and you say “where is the target?” Wherever the dart lands.
Now, this is the arrogance with which some doctors treat nurses. There is no fun for the nurse. Now if you have a target up there and I come in here throwing darts. Anyone will stop for a minute to see if you hit it. It's a challenge. It's tough on you if with you miss it all the time, to have that many people watching. But that's what education is all about. You want to improve after a while. Either that or you will stop publicly taking care of people, and that's an advantage too in some cases.
POMR 3.A - The Plan - Rule Outs & Investigations
Now, under any problem you put, A - what are you going to do firstand this is where you put ‘to more information’. This is the where you should always think about plans for the problem. This is where your rule outs go.I will rule out unilateral kidney disease. How? are you going to do it with a timed IPV, or a renogram? What are you going to do? And when that's done what are you going to do next?Aldosteronism - if so, you're going to do one serum potassium test or do five. Is the dividing line going to be 3.8, 4.3, 2.2? High salt diet or low diet.
Let’s precisely decide now before we spend your money.When you see doctors on work rounds saying, well, you know, we didn't get that-- see she had a little problem there, you know, she was a diabetic… I don't think I'm going to worry too much about that. No, that thinking should have been done before you drew it.
(33:10) When you see people thinking of what to do, and how to do it, and how they're going to interpret it, in 30 seconds at the end of a bed in a random fashion… It's like a contractor, all these architects they don’t mean anything, let's lay a few pipes here. No, you can’t do that. The pipes to the john will come up in the fireplace.
Now, fortunately, the human body can correct -- as I said to our house officers, “the sickest kidney is brighter than the brightest intern.” It will sort your IV's no matter what you do. But anyway, you have to put your rules out, see I have taken those rule outs away from the problem list. The problem list should not have rule outs, question marks, or probables. It should a precise reproducible statement of the problem at the level you can understand it and guarantee it. No matter how unsophisticated you have to get. We've got to fix the system so that students are much more ashamed of being in precise and dishonest than they are of being unsophisticated.They should never worry about whether they remember or whether they're sophisticated. All they have to be ashamed of is, “that I miscommunicated .”I overstated the case. I misstated the problem. As Bernando says, “the worst, the most corrupting of all lies, is to misstate the problem.”
So keep it pure and then in your plans under more information, goes your thinking and your logic. Don't let your differential diagnosis get mixed up with the problem, until you can update your problem in a secure way. I pick up charts, and it had infectious disease, question mark. Not a problem list. Now, what does that mean?
In our place I picked one up the other day that said, problem number 5, and rule out diabetics. I said what's the problem? He couldn't remember whether it was the urinary tract infection or if she was the one with polyneuropathy, he said you don't realize how busy this is, I said “doctor never lose sight of the problem”.I said, do you see what you would have done? You put rule out diabetics. You do a glucose tolerance, the resident says, how is that glucose tolerance? And you say, well, tolerance was 115 fine. We cleared that up she could go home. Cleared it up, she never had it.You see the problem is still vaginitis or neuropathy and the other plan was, rule out diabetics, and when that's normal what are you going to do next?
And you'll find if you do this rigorously that about half the time, on half of the problems you will never resolve it. You've got to learn what Whitehead talks about, it’s this capacity for sustained muddle-headiness. A tolerance of ambiguity. You know Pavlov said, “you must teach the graduate student gradualness.” He must never be forced to overstate his position. Misstate is a problem. Good medicine is a careful rigorous inching your way towards a more and more secure position.A final diagnosis is a myth.There are never two cases of lupus the same. There are no absolute final criteria. You must define them but recognize that it's the evolution and the following of a patient that is going to make the difference within these explicit definitions.
POMR 3.B - The Plan - Treatments
(36:40) All right. Now, what’s B on your plan? What you're going to do to treat never mix what you're going to do to treat with what you're going to do to get more information.Now you say, Oh, we never would do that. But yes you do. I’ll pull a chart and separate it and I see chlorothiazide. Now we're getting urine sodium for this aldosterone, and as I separate them… look, oh my God, you see what they were doing is, they were getting more information on what they did than on what they had. And we do that all the time. We do so much to a patient. We give them so many drugs and so many procedures and so much psychiatric confusion. Then when we do our test. It's really more information about what we've done to her, than what the original problem was. You know the intern gets her in and she's got all this diarrheaand next thing you know, he is doing stool analysis on barium.
POMR 3.C - The Plan - What you will tell the patient
Now, what's C, under any plan? What you're going to tell the patient? And no place in American records do we have an organized approach to what we're going to tell the patient.
Under that hypertension did you tell her it was serious or not serious? How are you going to study it or whether you're not going to study it? All right. Now, let me quickly get from the plan to the progress notes.
Never in American medicine have we highly structured progress notes in a problem-oriented way. Where we had a complete problem list and we numbered every progress note with respect to the problems.
Section 4: Follow Em
(38:33) So we're in this box 4 now. Never write, “doing well”. What does that mean? She's got arthritis, heart failure, azotemia, broken hip, ear infection and you put doing well. What you mean is, “I’m a cardiologist. They asked me to look at her, I did, we said digitalize her, I came in today, I listened, the rhales are gone away. The edema as left, she lost a few pounds. Gallop is gone away, rhythm a little slower, and her rates a little slower. I think she is doing well. I didn't know she had glaucoma. These urinary tract infections annoy me. I've never worked up a broken hip in 20 years anyway.” That's what he means by “doing well”. You know, someone said to James Thurber, “how is your wife?” “In what way”.
SOAP
Now, so you will always tile a number a progress note and you will always put the problem (1. Hypertension) and then always write symptomatically, objectively, your quick interpretation, your plan for the next step.
Always give the patient’s point of view first, then whatever objective data you have, and where you're going to go. So you're taking each problem in depth, and then you look back at the complete problem list and look at them in context.
Now, what does this mean? It means you can write a plan for azotemia, you can read Strauss's book or you can write one for heart failure, and here you can know about broken hips. But you can't write a book for Mrs. Jones who got this much heart failure and that much azotemia and a broken hip. She is absolutely unique. 88 keys on a piano and a million symphonies. There is no absolute treatment for anything. You can lay out your plan explicitly, set up your flow sheet, and then look at it, make a move like in the chess game, and then watch nature's move, then make another move. And you're a guidance system.
Now if you know those satellites, you see, they would get up there and they land here Wednesday or Thursday by this battleship. What are they doing? They're taking their position every instance with four computers on this system. And they keep re-adjusting their course. And the shape of the path is not precisely known until the input stops. It doesn't need to be known. But you have to know what your parameter of guidance, how often to look, and you'll re-adjust. When you go from Atlanta to Seattle. You never go to the same way twice. Sometimes you go the Northern route, sometimesthe southern route. Even if you try to go the same way twice, you could not. There's a red light here before there was a green light, the bridges washed out in Chicago, you read detour signs, and you go around. There is a tornado in you Montana. You meet a nice girl and you know, Oregon. You call up your family, you're going to be a couple days late. The car breaks down. But you know all the principles, red lights, green lights, detour signs, automobile maps. And once a boy has learned to go from Cleveland to Seattle, you don’t give a special course to go from Cleveland to Hong Kong, and Cleveland to San Francisco. You expect he will choose parameters. Same physiological ones over and over again. Whether you're having a fluid balance problem from heart failure, or a bad burn, or an intestinal obstruction, or diabetic acidosis. You're going to make volume decision, and a free water decision, and an acid-base decision and a potassium decision. It's the same heart and kidneys. The agent that through you off is a little bit different. But the commonality of it all has got to be seen by the student or her will memorize, and memorize, and memorize, and then collapse. Or just distort. It would be better. You know, what it's like in bio-chemistry. We get so upset with those flip-flops circuits when we do the counting. You wouldn't mind so much if they work or didn't work at all. But the problem is they half worked. And they sort of stopped counting in middle of the night. But you wouldn’t know it. And you would report something that was absolutely ridiculous.
That's the way interns and residents and doctors are. If they work perfectly it would be one thing, or if they didn't work at all. But we half work. We half guess. We half understand. We half know.
But we're never uncertain about going to the order book in writing a drug. No matter how busy a doctor is, I have yet to have a doctor say to me, ‘I was busy I didn't have time to order anything’. He's always so busy, didn't have time to find anything. But he's always got time to order something.
The M.D. Guidance System
(43:53) Now what I'm saying is, that a doctor has to be a guidance system. He is not an Oracle that knows answers. And once he accepts the concept of being a guidance system, then he knows that the data system is the basis from which all his work must take place.
And then the record suddenly becomes an unbelievably important document in education, in care, and in research.
But as long as we were a profession that thought we could rest on the memory. And it was what you know that makes a difference, instead of what you do. And as long as we thought of doctor's as Oracle that knows answers, instead of guidance systems, in uncertain situations.
We were willing to let the record in American medicine fall to this level.
And now when the computer people move in, and the Medicare people move in, and the non-medical people move in they can hardly believe what they see. And there is a crisis of major proportions.
The first hospital where I went, where we decided to stop source-oriented records, the first thing I did was we cancel all the conferences, and all the rounding that wasn't directed to specific problems. And from six in the morning till midnight, seven days a week, we got these things so the database was defined, the problem lists were up to date, the plans were in order, and there were progress notes at the right frequency.
It's just like a fifth-year graduate student in biochemistry when it gets down to the time, and he has got to get out, he stops going to hear the noble prize winners, he stops all these conferences, he stops running around, and he isn't going out to dinner with his wife, he isn't chatting in the hallway, he is doing one thing - he's in that laboratory, he's working on that thesis. And this [the record] is a doctor’s thesis. He may get A in all his courses. But if his thesis is no good, it's not creative, the work was no good, and it’s unreliable. All those A's in advanced calculus and biochemistry mean nothing.
And it’s the same with us. If this is not interpretable, or auditable, and the quality is not good, then all the rounds and all the specialization, all the NIH and all the hierarchy mean nothing. And then you might say, look but don't you think we should have research? Yes, I think we should have research. But this is research. Every patient is different, we don't have to run away from the bedside to be profound, and to be unbelievable scientist.
I worked a long time in biochemistry and nucleic acid chemistry and I can tell you from my own experience, and I was at Penn when the Meyerhoffs and all those people were there. And I've seen the best. And there's nothing that taxes you intellectually or taxes your sense of science and philosophy, the way this situation does.
Basic scientists would have been allowed to put focus on one or two problems, and keep their data in a separate notebook, and come in from eight to five, and shut off the incubator when they wanted to go away. They have no concept of what it is to have five problems per patient, 30 patients on the ward - 150 problems running simultaneously. They never taught a data system for that.
But because it's so difficult, and because it's just in its infancy of what we could do doesn't mean it's unscientific, or that its unsophisticated. And when someone says, “but oh jeez, isn't it more sophisticated to get new knowledge, or go to the NIH and work with Nuremberg, and find a new nucleotide or work out the code.” Well, those are pieces, there sophisticated, there worthwhile. I don't begrudge him his noble prize. I'm glad to have these things happen. I've worked on these. I got more money and more job offers and more professorships offered in biochemistry, then I ever did in clinical medicine. And I don't begrudge people for that. It was very useful to me at the time.
But to say, that the sit up in the attic, carving the chessman, and writing the rules - as the university has done for 2000 years - to say that is more sophisticated than playing the game with those men; that's ridiculous. It's unbelievably sophisticated to take those men and play the game. And you don't need to stop making the chessman. We don't need to burn down the NIH or stop the research laboratories. To go on to this more sophisticated state of playing.
So the students should never think of that clinic with hundreds of patients and all this confusion and how to get the database - that's a very sophisticated problem, in systems analysis, in efficiency.
In order to decide if you've got 100 patients to see there this afternoon, and you've got to get the database that will yield most, which problems do you want, you've got to know a great deal about the science of medicine. If we’re after heart failure is it best to have venous pressure? Ask five questions on the history. What is the highest yield? If it is hyperthyroidism, should we talk to her about diarrhea, weight loss, should we grab PVI'S? If there are 10 things you could do, which has the highest yield? What do they really know about hyperthyroidism anyway? Let's turn it to play this game. And you'll find that they haven't really thought about very rigorously. They just have the pieces. They're going to put them together tomorrow. But tomorrow never came.
And of course, you know, Pusey said but isn't the university to discover new knowledge? Of course, University is to discover new knowledge. But the new knowledge we need now, and it's most difficult and most sophisticated, the new knowledge we need now is how to use knowledge. That's a very profound thing to do.And this [the record] is the physical representation of doing or not doing it. And it runs head-on with society.
Now it’s very easy to go down to the molecular level and work with trinucelotides and triphosphates or anything else. Or to go out into outer space, where only your methods can measure how badly off you are. In biochemistry, we use to say we have microsomes and the mitochondria, that's a pure mitochondrial prep we would say. We thought it was until, the methods got better and we could see it with the electron microscope, and see it full of junk. Microsomes all sorts of junk in there. In other words, the purity of these isolated systems is only as good, as so far as your capacity to find the faults.Whereas when you work in that clinic, it's at the macro level, it's not so distant and so macro that you can't see it. It’s not so micro that you can't see it. Its patients moving around. It's like a big cell here. And instead of mitochondrial, it's actually patients and doctors and pharmacies. And there's a nucleus. It can be centrifuged and separated and put together and studied.
But the reason we don't like to do it is because your faults are so obvious. Your mistakes are so obvious. The lack of purity of your approach is so obvious. You can't stand it, so you say it's “unimportant” or “is not scientific” or “that not why I came into medicine.” Your cowards. It’s perfectly clear that's what the problem is. Society is unreasonable.It's frustrating, it’s irrational. The cell was too, the centrifuged was too. Those mitochondria were too - they weren't pure preps. The only difference was they couldn't talk back, and we couldn’t see it. And we didn't device methods to see how badly off we were.
Conclusion - ‘the art of medicine’
(51:55) All right. Now, let me make one a closing remark about what this has got to do with the art of medicine. Where is the art of medicine going to go with all of this, if you have lists and numbers?
Well, art is style, structure, form, discipline. It’s Andrew Wyatt making Jamie Wyatt do the painting 50 times until it’s right. Unbelievable discipline about technique. He made that boy tear up a painting a 100 times. It’s George Szell, if you have ever watched him with that orchestra - the same passage 30 times until it was perfect, and no violinist stood up and say, “this interfering with my art”. Nor did Bach say, “three beats in every measure, oh that's going to interfere with my creativity, that's too like an old maid”. No, art is Hemingway three weeks on a single paragraph. Its Bach recording in detail everything he did a couple hundred years ago so we can hear it today.
It's not a scribble in the middle of the night. It's not saying I took good care of her, leaving absolutely no trail for us to ever find out if you did or did not. We debase the word art itself when we call what we've been doing art… And it's not science, so we have to extremely be careful when we defend what we're doing… We don't reveal to others that we didn't even get out of a liberal arts education, Stravinsky says, ‘art is nothing more than placing limits and working against them rigorously’…And if you refuse to place them, and try to work within them, but flayed out. You do not have art. You have chaos. And to large extent, that's what we've had.
Thank you very much.
/transcribed with assistance